Covid-19 Christmas 2021
An unwelcome visitor this Christmas
At 8am Christmas morning the phone rang. “Mum, I’ve just tested positive for Covid”.
The previous night, a close friend told me her daughter had tested positive, and their household would be in isolation with her for at least the next week.
Despite having taken all the health advice of social distancing and getting vaccinated, the pandemic suddenly shifted from being a lockdown inconvenience to an immediate health issue affecting our loved ones.
Living “with” Covid-19?
Earlier in the year, while working and studying from home, we watched the 11am NSW government updates in dismay, hearing about daily case counts in the hundreds and young people getting sick with Covid-19. After nearly two years of living with intermittent lockdowns (including the mental health, education and business impacts), vaccine debates, social distancing, mask wearing and the ongoing fear of contracting the virus, we have been conditioned to fear Covid-19.
However, going into Christmas with NSW daily counts hitting several thousands and without our familiar protections of masks and QR codes, many of us were wondering whether the current leadership was blind, stupid or brilliant. We were very concerned to learn that our daughter and our friend’s daughter were sick with Covid-19.
While my daughter has been very sick, at the time of writing she seems to be improving and recovering at home without complications. Here’s what we learned from the experience:
There are real people behind the numbers
Case numbers are people
As an actuary, I’ve spent most of my professional life looking at numbers. However, many of us are now regularly following the statistics on Covid-19 on a daily basis. For some excellent analysis and commentary on Covid-19 statistics, see Jennifer Lang’s extensive blog.
But while our current leaders are urging us to focus on hospitalisations rather than total cases, it is important to remember that every “Covid-19 case” is a real person who is unwell to some degree. They are a friend, partner, parent, child and/or sibling to others who will be concerned and may be also at risk of getting sick. This is not just about sterile numbers, this is about people.
Remember the person
With new daily case numbers so high[1], there is a greater chance than ever before that you or someone you know will test positive for Covid-19. Remember that they are a person, and try to ask “Are you ok?” and “What do you need?” instead of (or at least before) asking questions such as “Where did you get it?” or “Could you have infected me???”. The person who has received the result is likely to be unwell and worried.
Health before politics
With so much political charge around the situation it can be easy to forget we have an increasing number of very sick people who need various degrees of support. The current demand on the health system (that is doing a stellar job given the circumstances!) means that caring for people with Covid-19 will primarily fall to their families and friends. Due to the infectious nature of the disease, we need to protect ourselves AND care for those who are unwell. We sought advice from the national HealthDirect helpline (1800 022 222 – an excellent resource) about how to best keep this balance, which included providing regular welfare checks and healthy food, while visiting outside, keeping a safe distance, correctly wearing and disposing of masks and hand sanitising. While most people are expected to safely recover at home, 000 is always available in an emergency.
What we are doing well
Vaccines seem to be working
I am not medically qualified, and I have had difficulty finding up to date data on case statistics by vaccination status, but based on the proportion of cases requiring hospitalisation[2] it appears that increased vaccination rates are linked with lower hospitalisation rates.
My daughter was double vaccinated but still caught the virus and was quite sick, but health advice suggests that she may have been sicker without having had her vaccines. Her partner lives with her, cared for her at home while she was sick, and was also double vaccinated, yet has not caught the virus. Her friends who saw her the night before her positive test are all double vaccinated and didn’t get sick. My friend, whose daughter tested positive on Christmas Eve, shared a single bathroom and house with her and her family – all double vaccinated - in household-contact isolation for a week but no-one else got sick. In our small sample it appears that vaccination may have protected close contacts from contracting Covid-19 from our daughters.
Health care workers are amazing
Having now cared for a family member sick with Covid-19, I think that the only thing worse would be having to care for people sick with Covid-19 every day. The medical staff on the frontline surely didn’t expect to work through a pandemic when they chose their respective occupations.
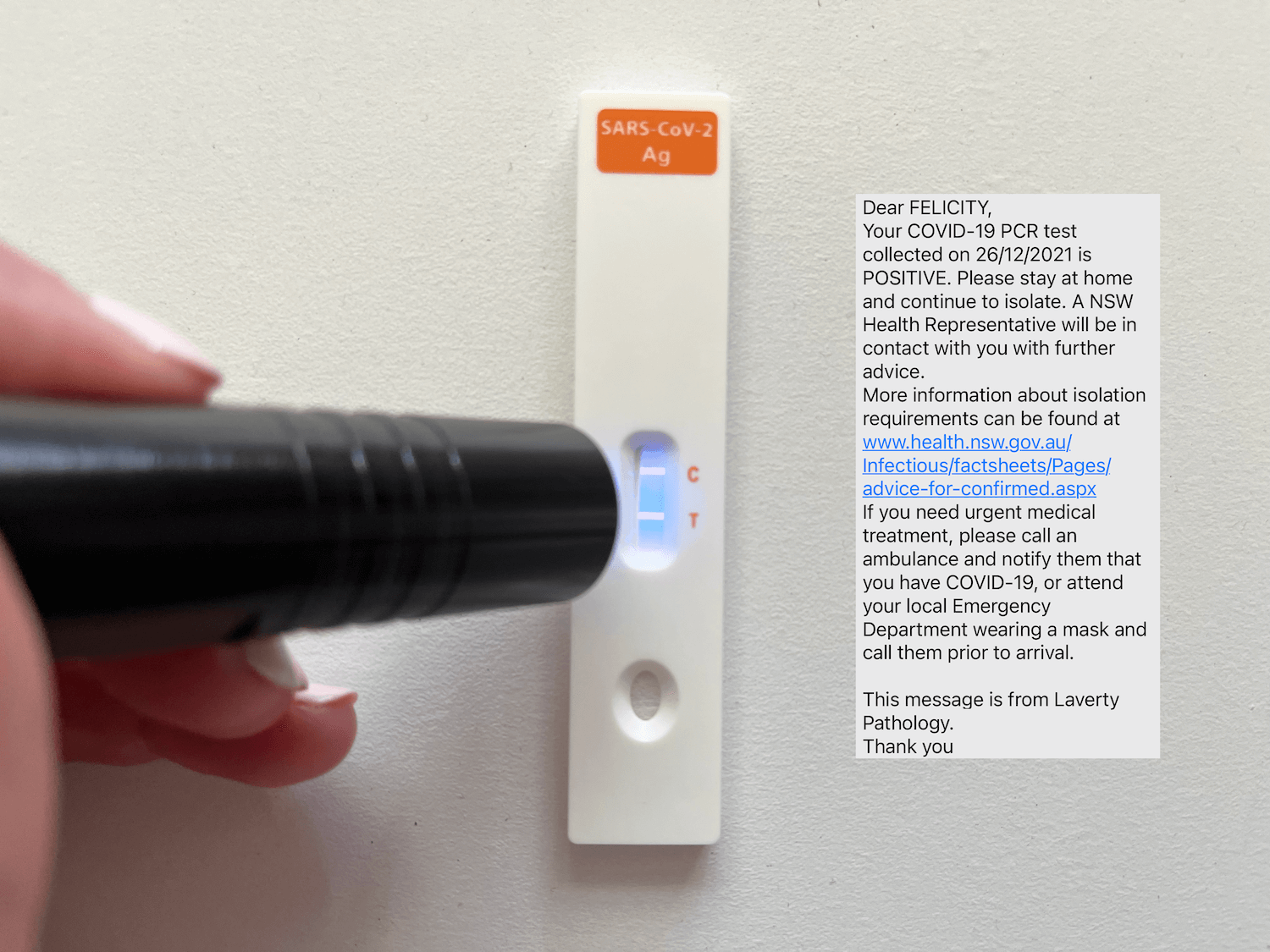
Following her positive Rapid Antigen Test (RAT) on Christmas Day, my daughter attempted to get a Polymerase Chain Reaction (PCR) swab test at the local hospital. However, by the time we reached the long queue at 9:10am (ten minutes after they opened) we were turned away. I begged the nurse for a test and advice, telling her my daughter was symptomatic and had a positive RAT. However, the nurse (giving up her own Christmas Day to test cranky and sick locals) said that while they were at capacity for tests, to go home and isolate, try again tomorrow and call the public health unit for information and 000 if there’s an emergency. This was the best outcome with the current policy and practice in place, and I was grateful that she took the time to speak with me.
Christmas morning queuing for a PCR test
What we need to do better
Accepting higher case numbers means the system must change
If our leaders choose to accept a higher number of cases, the system needs to have the capacity not just to manage hospital admissions, but to support timely testing and appropriate health care for all people with Covid-19.
The first in – first served testing centre approach works when there is sufficient capacity for everyone to get a test when they need one, even if they have to wait a little while. However, it is not equitable or safe for people to have to queue while sick for up to 5 hours, or wait until tomorrow or the next day because they’ve been turned away from today’s testing centres. Additional capacity and a testing triage approach could help reduce unnecessary risk of transmission.
Clear isolation and testing rules
We shouldn’t need a degree in actuarial science or medicine to work out how to follow the isolation and testing rules. What if I couldn’t get a test for 3 days after I got sick? When is “day 6” for my household contacts if my test result took 5 days to come through? Am I really a close contact if someone has only had a positive RAT? With the delays in testing, how many infectious people are living and working in our community unable to confirm their Covid-19 status? When can I leave isolation after I’ve recovered from Covid-19? Do I need medical clearance? When the advice is updated, does this apply to everyone who is currently sick, or just those who are yet to test positive? What if I must isolate for 7 days but I don’t have sick leave? The answers to these questions are not always consistent, clear or easy to ascertain.
Recent advice in the US[3] suggests that transmission is greatest up to 2 days prior to, and 3 days following, the onset of symptoms, hence recommending a 5 day isolation period after a positive RAT. The current rules work when we have a testing system that can meet demand, or at least wide availability of RATs (anyone found any over Christmas???). We need some evidence based, clear and consistent rules around isolation and testing, and this should apply to all Australians in all states.
Daily counts are not robust evidence
Our leaders continue to remind us that they are reviewing “the evidence” and making decisions based on that information. I wonder if they have additional information that we aren’t privy to? It is a common trap when interpreting numbers that somehow by quantifying something it must be accurate. Daily case counts tell us about known infections from several days ago, but over Christmas the day-today case counts will be impacted by delays from people getting tests and from labs processing tests. With increasing proportions of positive test results, we may not have representative samples of tests and therefore many additional cases are missed in the official statistics. Trends in daily counts give us a sense of magnitude, but care should be taken when focussing on daily counts as “evidence” for policy changes.
Missed opportunities for data collection
Due to higher case numbers, we cannot conduct the same level of contact tracing as was performed earlier in the year. We are also missing an opportunity to collect data from people who are sick with Covid-19 at home, which can help us better triage people needing support and also help us make decisions about future variants and outbreaks.
When my daughter finally received her positive PCR result, five days after she had symptoms and a positive RAT (despite her best efforts while very sick to get a PCR test), NSW Health sent her opt-in style text messages. They asked her four questions – around overseas travel, why she got tested (and a positive RAT was not an option!), whether she’d recently visited any high risk settings and whether she identified as Aboriginal or Torres Strait Islander. No information was collected about her vaccine status (which theoretically could be linked with other Medicare data, but we data nerds know that sounds easier than it actually is) or her severity of illness, symptoms or level of support available to her. QR code check-ins were abandoned and reintroduced prior to Christmas, but gone are the days of tracing the source of every case.
A move to RATs over PCR testing appears to be a sensible option with the current PCR bottlenecks, but this would also reduce our data collection (unless there is a mechanism for people to provide their home RAT results) and increase the risk of transmission if people cannot afford or access a RAT, or choose not to take one. If policy decisions are based on RAT testing, we need clear guidelines for provision and regulation around test results.
We have a missed opportunity to collect more data to help us triage and provide appropriate health responses now, and to inform a better response next time.
Financial support is needed
Financial support for those required to isolate, as well as provision of free personal protective equipment and RATs will be needed to protect our community. The new Lessing family household budget line item “masks and hand sanitiser”, with a recent update to include “RATs”, is manageable as we can afford to pay for this protection. When I was a teenage mother, rationing bread and making powdered milk to stretch the weekly grocery shop, these items would have been unaffordable, as they will be for many people in our community today. Consideration of free masks and hand sanitiser for those on health care cards or welfare could reduce the risk.
Higher cases mean there’s a higher chance of needing to isolate for 7 – 10 days, whether you are sick or a close contact. Not everyone has access to sufficient sick leave to cover these periods. Particularly since the largest age group affected is young people aged 20 - 29[4], who are more likely to be on lower incomes and casual workers, income support would help these people and reduce the pressure on them to continue working while sick.
We need to do more - NOW
While the frontline health workers are doing a stellar job and vaccination rates appear to be linked with lower hospitalisation rates, there is more we need to do if we are expecting the community to “live with Covid-19”.
Remembering that every case relates to a human being, who may experience a spectrum of symptoms whether vaccinated or not.
With the rising case numbers and an under-resourced testing system, we all need to know how to safely care for friends and family who contract Covid-19.
We need to increase capacity or introduce triage procedures to safely and efficiently test and support those who are most likely to be sick with Covid-19, while reducing the risk of transmission during testing.
We need free and accessible RATs, as well as free or affordable masks and hand sanitiser for those on low incomes.
We need a provision for income support for those who contract Covid-19 or who are required to isolate, to support those affected and reduce the risk of people returning to work while infectious.
We need clear, consistent, evidence-based testing and isolation rules that apply to all Australians.
We must remember that daily case numbers are not necessarily robust for decision making purposes, particularly when there are delays in testing and lab results.
We need to take the opportunity to gather the right data, when people test positive and if we move from PCR to RAT testing, to help prioritise support for those who need it most and prepare ourselves for the next outbreak.
Stay safe and be kind.
As case numbers continue to explode, some of you may have had a similar experience this Christmas. If you or your loved ones have contracted Covid-19, I send you my best wishes for a speedy recovery. Stay safe (if you can).